How ‘Smack City’ Liverpool halted an HIV epidemic

1980s Britain was an era of deep social unrest. As the effects of a new, Thatcherite government ripped through the country’s working-class towns and cities, a series of interconnected public health crises began to emerge from the rubble.
Before then, heroin use had been for the upper and middle-class yuppies – the types who never seemed to find themselves in Class A-related trouble. But, as unemployment swept the country, a new type of heroin arrived on the scene, and with it, a new demographic of drug users.
Brown heroin was cheap, and arrived in Merseyside at a time when unemployment in Liverpool had exceeded 20 per cent – double the national average. With 20,000 drug users out of a population of two and a quarter-million people, Liverpool was branded ‘Smack City’. At the same time, an ominous public health crisis was simmering in the country, having already scourged America: HIV.
As per Russel T Davies’ poignant Channel 4 series, It’s A Sin, HIV was dismissed by an intolerant and frankly homophobic public as a gay man’s disease. But data from New York City showing that around 80 per cent of intravenous drug users were HIV positive suggests otherwise.
This is the story of how public health officials in Liverpool pioneered a harm reduction approach to drugs and public health, and how a city crippled by heroin use was able to avoid an HIV epidemic among injecting drug users.
The perfect storm for a public health crisis
Andrew Bennett (Joint Drugs Service Manager): In 1984, I was appointed as a youth worker on the Cantril Farm estate (now called Stockbridge Village) to engage with unemployed young people, 16 and above, which was the majority of unemployed people at that time. In the end, most of the work revolved around drugs because, as I arrived, brown smokable heroin arrived on the estate.
Carol Hill (Outreach Worker): The unemployment was horrendous. Nobody had any money. You couldn’t afford to go out drinking and stuff like that. It was boring. The quickest way to get through it was for people to get high, however they could.
Lyn Matthews (Outreach Worker): [Unemployment problems] came in combination with a pot drought. Kids would go to dealers on the estate to get pot and would be offered ‘brown’ instead. They didn’t know what it was so they got into it. Next thing they knew, they had a habit.
Pat O’Hare (Adviser on Drug Education): I was a teacher in Bootle at the time. We had kids in school who were chasing the dragon, getting into trouble. They used to come to me with their problems, and increasingly they’d come with their bloody drug problems.
We had one kid, he was an amateur boxer. I said, ‘Come on, box me!’ and before I got my hands all the way up, he’d hit me. He was so fast! But he overdosed and died when he was 17.
Alan Matthews (Editor of the Mersey Drugs Journal): We first heard about HIV through medical reports from the USA in 1985. They were talking about this weird virus called HTLV-III, which was killing gay men in San Francisco and drug injectors in New York City.
So we got in touch with counterparts in public health in New York, and said, ‘Why has this spread so fast?’
They said the police could arrest you if you just had syringes, so people were sharing needles. That’s why we thought, hang on, we need to loosen up our drug policy and make sure that clean needles are readily available to people.
Carol: I’d had a partner who was a long-term injecting drug user when I was younger, so I knew what it was like from that side of it. They had to share their injecting paraphernalia.
I know people that lost limbs because they were injecting and they didn’t have clean needles. If [a dirty needle is] the only option for them, that’s what they were using.
A radical push towards unconditional public health
John Ashton: I was working as a public health consultant with the Mersey Regional Health Authority with Howard Seymour, the first regional health promotion officer for Merseyside, developing health promotion initiatives.
Howard and I were at a conference in Dublin in 1985 where we met Glenn Margo. Glenn was one of the public health directors in San Francisco and he was a gay man who was HIV positive. We heard him talking about the situation in San Francisco, and we invited him to Liverpool to share his experience with everyone there.
Towards the end of his stay, we asked him what he would have liked to have done differently back in 1980 when the cases of AIDS first started to appear in San Francisco, and he said, ‘You’ve got to work closely with people themselves, you’ve got to work with them as partners, and you need to work with the gay community, and you need to do syringe exchange.’
Andrew: I was working as a drugs counsellor at Sefton Council. I argued to my manager that we weren’t going to stop HIV with counselling. We needed population-based approaches [an approach to health that aims to improve the health of the entire population rather than in individual patients]; we needed to set up a syringe exchange scheme.
It was at loggerheads with the council in Liverpool, who argued vehemently that this was the wrong way to go. Some of the leaders in the council thought we were condoning drug use by not being tough on drugs, by not saying don’t do it, by not saying drugs are bad. So everything that was achieved in that first really important five years was achieved without the support of the council.
John: For context, it was during the Thatcher government. It was really quite prudish and puritanical. The idea of doing syringe exchange was difficult.
Alan: The thing is, if John Ashton hadn’t been in the upper echelons of public health, we wouldn’t have been able to do it.
Now, all the moral aspects of whether people should use drugs or not had nothing to do with it. There was a higher kind of reason for doing this, and that was to protect public health. Because of course, people who inject drugs don’t just inject drugs with each other. They have sex with other people. And that’s how it was going to get out into the broader, non-drug-using community. John and Howard recognised that, and they convinced Sir Donald Wilson, who was the chair of the Regional Health Authority.
John: We arranged to do [the syringe exchange] on the basis that we wouldn’t go public about it. This was coming up to Easter 1986. So, Howard went and found the building on Maryland Street, and we arranged to get started with Allan Parry (a former drug addict who was director of the new Mersey Drug Training and Information Centre).
We worked closely with the police – the vice squad and the drug squad – and the churches. We also had support from the editor of the Liverpool Echo, and we agreed they wouldn’t write anything about it in the paper until we were ready.
Pat: The police were great. Derek O’Connell (head of the drug squad) said, ‘We have a role in ensuring public order, but we also have a role in public health’. So they agreed not to come near the service on Maryland Street. And if you’ve got the police on your side, when you’re talking about illegal drugs, it’s pretty big.
Alan: One group we didn’t consult was the parent support groups [for parents of drug addicts] because we knew they would be opposed to it.
Carol: There was a massive battle at first with the parents of these young children and of heroin addicts. Because we had a massive problem in Merseyside around that time, the thought of them being able to get syringes and needles whenever they wanted to frightened parents.
Andrew: I did a lot of talks with different community groups and parents groups. They were worried, and it was about trying to understand people’s fears and explaining why we’re actually with you on this – we’re trying to prevent harm and trying to keep your son, your daughter safe.
Alan: We ran the needle exchange as a pilot without any publicity, just word of mouth on the grapevine. We ran it for six weeks to see if anyone’d sign up. In six weeks, 300 people came to Liverpool because they’d heard about it off their mates.
John: It took off. There were, around six or seven hundred people within a few months.
In the summer of that year, the news broke that in Edinburgh, police had been very heavy-handed with people who had syringes in their possession, and they would be prosecuted. So drug injectors in Edinburgh were using shooting galleries and sharing equipment. Something like 30 or 40 babies were born HIV positive.
Andrew: There was a very famous report published in 1987 by the Advisory Council on the Misuse of Drugs. The key finding was that HIV was a bigger threat to individual and public health than drug use was.
John: I was very close to the Chief Medical Officer for England, Sir Donald Acheson. When all this was happening in Edinburgh, Donald said, we need to have some pilots of syringe exchange [around 15 other syringe exchange programmes were rolled out around the country to test whether this approach would help stifle the spread of HIV, and the Maryland Centre became an official part of that scheme]. So, at that point, we put our hands up and said ‘Can we be a pilot, please, because we’ve been doing it for six months?’
The rest is history.
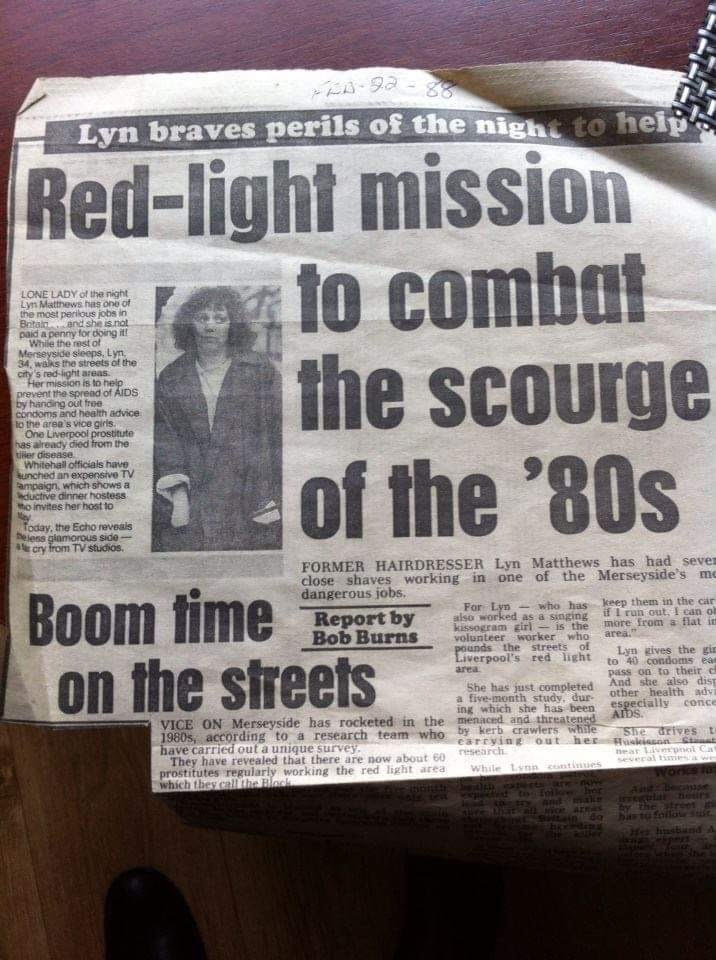
Courtesy Lyn Matthews
The inner workings of a harm reduction approach to drugs
John: The principles [of the need and syringe exchange] were to make contact with drug users and other vulnerable people, to maintain contact with them and to make changes to their habits as and when people were ready to do so. So the whole argument was, there’s no point trying to do anything unless you make it easy for people to access you and you’re not judgmental.
Andrew: It became, in some respects, like a primary healthcare service for injectors. So it was initially clean syringes, clean needles, leaflets and some advice. Then nurses were employed, who were very sympathetic and whose attitudes around drugs didn’t hold them back, and users were getting general healthcare that they would have found difficult to access elsewhere. We would see people with poor health, abscesses, loss of limbs. They were really ill, because of complete neglect and difficulties in accessing services.
Lyn: If some injecting sites were bad, users could go away with dots on their groin to show where to actually put the needle in safely. People stopped getting leg ulcerations and deep vein thrombosis because we had a nurse who’d chosen to do that.
Carol: There was a big push to get people onto methadone around that time, as an alternative to heroin. It was a medicine so they didn’t have to inject it. That really helped.
Alan: Of course, not everyone is going to come into the health authority, through fear. We knew there was a group of people working down the road by the cathedral, selling sex. Hardly any of them came to the needle exchange.
One or two of them did. These were older injectors that had known Allan Parry, and people working with us. We were saying to them, ‘Why don’t all the girls come here and get free condoms, free needles, if they need them?’
And they were like: ‘Well, you’ve gotta walk past Hope Street Police Station to get here.’
[It was illegal under the Sexual Offences Act 1956 for street prostitutes to “loiter” or solicit in a street or public place for the purpose of prostitution. It was also illegal for men to “kerb crawl,” and solicit sex from street prostitutes].
I was a youth worker in the ‘70s. And for those kids that didn’t come to the youth club, you took the youth club out to them. You engaged with young people where they were.
So we thought, what we need is somebody to do detached needle exchange work. We need an outreach worker. And it’s going to take a particular type of person to be able to go out on those streets and engage with these women who were marginalised in every sense you can possibly think of.
They’ve got to be dead hard, they’ve got to be bare-faced, they’ve gotta have a big gob, they’ve got to be engageable, they’ve got to have balls of steel. And I said, ‘Yeah, that’s my wife.’ [Lyn]
Lyn: Through my outreach work with the women, the actual amount of women attending the drug dependency unit went up something like 37 per cent.
Laura* (Ex-Sex Worker): I started using the clinic on Maryland Street because Lyn Matthews would run me down. She used to hound me, but I think she took me under her wing.
A lot of the girls had an issue with trust. But, after a few attempts, I took to her. That’s when I started going there, getting condoms and listening to Lyn give advice.
Andrew: None of us were trained, really. There was a very limited amount of professionalisation in the fields then.
Carol: I had experience of drugs, you see, and of knowing injecting drug users. Because I knew people, and I knew what I was talking about, people found it much easier to open up to me, rather than a nurse or somebody official.
Lyn: I think having that experience [of recreational drug use] was important, and being able to switch between talking to people on a street level, and then on a professional level. It’s quite skilled.
Drug users can tell instantly if you’re judging. They know the ones who genuinely care and the ones who are just doing a job. They also know who knows what they’re talking about. Being able to speak in their language is really important. So is being transparent.
Carol: I had to do a lot of work on gaining trust. I don’t think anyone would have even spoken to me if I hadn’t been like them. I’d have been run off the estate.
Lyn: I knew loads of people in Liverpool who were sex workers, and I was very familiar with the area, so I wasn’t scared. But what we did was actually quite dangerous, because I was mixing with gangsters, high-level drug dealers and all different kinds of people.
Outreach workers were like the dustbin men of the drugs field at the time, but doing that frontline work, you have to be highly skilled.
The results: Was the Mersey Model a success?
Andrew: There was not an epidemic of HIV amongst injectors [in Mersey], I think, through the prescribing of methadone and advice and leaflets. They were very important things that helped to protect people from harm. We were successful.
John: There was quite a dramatic difference actually, between Liverpool and the other cities, in the percentage of intravenous injectors who were HIV positive.
The proportion of injecting drug addicts who were HIV positive in 1991 in the UK was one in 4.3, so around 25 per cent. In South West Thames, it was one in 18.8.
In Mersey, it was one in 82.4.
Alan: If we hadn’t had done what we’d done, thousands and thousands more people would have died.
Follow Ella Glover on Twitter.
Enjoyed this article? Like Huck on Facebook or follow us on Twitter.
Latest on Huck

Clubbing is good for your health, according to neuroscientists
We Become One — A new documentary explores the positive effects that dance music and shared musical experiences can have on the human brain.
Written by: Zahra Onsori

In England’s rural north, skateboarding is femme
Zine scene — A new project from visual artist Juliet Klottrup, ‘Skate Like a Lass’, spotlights the FLINTA+ collectives who are redefining what it means to be a skater.
Written by: Zahra Onsori

Donald Trump says that “everything is computer” – does he have a point?
Huck’s March dispatch — As AI creeps increasingly into our daily lives and our attention spans are lost to social media content, newsletter columnist Emma Garland unpicks the US President’s eyebrow-raising turn of phrase at a White House car show.
Written by: Emma Garland

How the ’70s radicalised the landscape of photography
The ’70s Lens — Half a century ago, visionary photographers including Nan Goldin, Joel Meyerowitz and Larry Sultan pushed the envelope of what was possible in image-making, blurring the boundaries between high and low art. A new exhibition revisits the era.
Written by: Miss Rosen

The inner-city riding club serving Newcastle’s youth
Stepney Western — Harry Lawson’s new experimental documentary sets up a Western film in the English North East, by focusing on a stables that also functions as a charity for disadvantaged young people.
Written by: Isaac Muk

The British intimacy of ‘the afters’
Not Going Home — In 1998, photographer Mischa Haller travelled to nightclubs just as their doors were shutting and dancers streamed out onto the streets, capturing the country’s partying youth in the early morning haze.
Written by: Ella Glossop